
Introduction
Known as the ‘English Disease’, rickets, or for adults, osteomalacia, is a vitamin deficiency disease that causes the softening of bone. It was discovered in the early twentieth century that the cure to rickets was a newly discovered vitamin, called vitamin D1. Vitamin D functions in calcium and phosphorus absorption from the gastrointestinal tract. These minerals are used in bone mineralization, creating strong bones and curing soft bone diseases.
Vitamin D is a powerful epigenetic modifier. That is, vitamin D has been shown to activate or suppress more than 2,500 genes. Vitamin D covers health issues such as cancer, chronic inflammatory diseases, diabetes mellitus, acute respiratory tract infections, and multiple sclerosis2.
Where does vitamin D come from?
Vitamin D is difficult to obtain in sufficient quantities through diet alone. Most of vitamin D is obtained when our skin converts ultraviolet light (UV) into vitamin D. It makes perfect sense that you would find vitamin D deficiency in Scotland considering its high latitude limiting UV sunlight exposure to little more than three hours a day on a yearly average.
How could anybody make do with such little UV light? Well, it turns out that skin color3 controls how much UV light is absorbed. The more melanin pigment present, the darker the skin color. Melanin functions to absorb UltraViolet Radiation (UVR), protecting the underlying skin from damage. Therefore, there is a tradeoff associated with the amount of melanin pigment present and levels of vitamin D. While darker skin is more protective against skin cancer, this added benefit reduces the amount of UV light used to produce vitamin D. However, those with lighter skin have the opposite, where more vitamin D is available while skin cancer is more common.
This again makes sense when you look at a skin color as a function of latitude. Those living closer to the equator have darker skin protecting them from the intense UVR, while those living in Scotland have much less melanin pigment to help attain what little UVR they can get.
Vitamin D2 vs D3?
You’ll see vitamin D on the shelves as either D2 or D3. The difference is that Vitamin D2 (ergocalciferol) is plant based, while vitamin D3 (cholecalciferol) is sourced from animals. The recent literature4 shows that D3 is more effective in optimizing vitamin D status.
Where are the vitamin D receptors?
Since vitamin D’s discovery in the early twentieth century there have been many more functions identified other than gut mineral absorption. While vitamin D was originally considered to relate exclusively to skeletal health, research has shown calcitriol (the active form of vitamin D) metabolism by immune cells and lung epithelial cells.
Receptors for vitamin D can be found in the intestine, pancreas, prostate, and immune system. More interestingly, vitamin D receptors are found in almost all immune system cells. Including: T cells, B cells, natural killer cells, dendritic cells, and monocytes/macrophages. Indeed, vitamin D is no mere vitamin, rather it should be regarded with the same importance as other steroid hormones.
What is the specific metabolic pathway of vitamin D?
Structurally, vitamin D is very similar to steroid hormones such as estradiol, progesterone, testosterone, and cortisol. Basically, after sunlight contacts our skin, and a few transformations in the liver and kidney, we can use vitamin D.
Figure 1 below illustrates this mechanism in more detail. The metabolic pathway5 of vitamin D begins with UV-B (light at wavelength 280-315 nm) exposure converting 7-dehydrocholesterol to cholecalciferol in the skin. The cholecalciferol is transported to the liver where it is hydroxylated, creating 25-hydroxycholecalciferol (also called calcidiol). Essentially, hydroxylation is the process of adding an OH group to a chemical. These forms of vitamin D are all inactive until one further hydroxylation step leading to 1,25-dihydroxycholecalciferol (calcitriol), the active form of vitamin D.
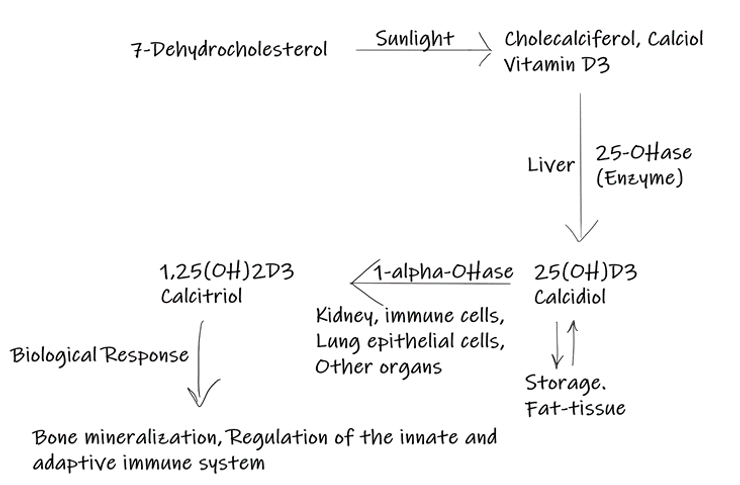
Figure 1. The metabolic pathway of vitamin D
What is the relationship between the SARS-CoV-2 virus and vitamin D levels?
Vitamin D plays an essential role in regulating the innate and adaptive immune system6. The innate immune system is the body’s first line of defense against pathogens while the adaptive immune system provides a much more specific immune response carried out by white blood cells.
It is well known that vitamin D supplementation protects against acute respiratory tract infections (ARDS)7. With vitamin D playing a protective role against respiratory disease, its remedial benefits associated with the SARS-CoV-2 virus is no surprise.
Following a systematic review5 of the current research as it relates to vitamin D and the SARS-CoV-2 virus, published in Nutrients on October 14th, 2021, a specific interaction exists between vitamin D and the SARS-CoV-2 virus.
Acute respiratory disease syndrome (ARDS) and cytokine release syndrome (CRS) are the most life-threatening stages during a SARS-CoV-2 infection. ARDS and CRS activate a large inflammatory response that causes the most damage in severe covid cases. Vitamin D inhibits the metabolic pathways underlying ARDS and CRS.
In more detail, this all occurs in the renin-angiotensin system (RAS). In this system there exists a delicate balance between angiotensin II and angiotensin-(1,7) where angiotensin II is pro-inflammatory and angiotensin-(1,7) anti-inflammatory. The ACE2 receptor converts angiotensin II into angiotensin-(1,7), controlling the balance.
It just turns out that this ACE2 receptor is the main receptor for SARS-CoV-2. This leads to a decrease in angiotensin-(1,7) and an increase in angiotensin II. High angiotensin II levels lead to ARDS and then severe Covid cases. Vitamin D inhibits angiotensin II synthesis and promotes ACE2 production, decreasing the inflammatory response, thus decreasing the severity of the infection. There exists a causal relationship between vitamin D blood levels and SARS-CoV-2 severity.
This systematic review paper selected eight eligible studies that recorded vitamin D levels and Covid mortality rates. Quantitative analysis among these studies showed a median vitamin D level over all cohorts of data to be 23.3 ng/ml. The linear regression line illustrates that in theory Covid morbidity approaches zero at a vitamin D blood level of 50.7 ng/ml.
Interestingly, the 50 ng/ml recommendation made by this paper matches the vitamin D levels found in those with more traditional hunter/gatherer lifestyles8.
The recommendation of 50 ng/ml is much different than that of the CDC’s and WHO’s which are both around 25 ng/ml.
Disclaimer – I am not a Doctor. Consult with your primary care giver for questions regarding what’s best for you.
- Deluca, Hector F. “History of the discovery of vitamin D and its active metabolites.” BoneKEy reports vol. 3 479. 8 Jan. 2014, doi:10.1038/bonekey.2013.213
- “Multiple Sclerosis: Lipids, Lymphocytes, and Vitamin D.” Immunometabolism, 2020. DOI.org (Crossref), https://doi.org/10.20900/immunometab20200019.
- Webb AR, Kazantzidis A, Kift RC, Farrar MD, Wilkinson J, Rhodes LE. Colour Counts: Sunlight and Skin Type as Drivers of Vitamin D Deficiency at UK Latitudes. Nutrients. 2018; 10(4):457. https://doi.org/10.3390/nu10040457
- Tripkovic, Laura, et al. “Daily Supplementation with 15 Μg Vitamin D 2 Compared with Vitamin D 3 to Increase Wintertime 25-Hydroxyvitamin D Status in Healthy South Asian and White European Women: A 12-Wk Randomized, Placebo-Controlled Food-Fortification Trial.” The American Journal of Clinical Nutrition, vol. 106, no. 2, Aug. 2017, pp. 481–90. DOI.org (Crossref), https://doi.org/10.3945/ajcn.116.138693.
- Borsche, Lorenz, et al. “COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 Ng/ML 25(OH)D3: Results of a Systematic Review and Meta-Analysis.” Nutrients, vol. 13, no. 10, Oct. 2021, p. 3596. DOI.org (Crossref), https://doi.org/10.3390/nu13103596.
- Wei, Ran, and Sylvia Christakos. “Mechanisms Underlying the Regulation of Innate and Adaptive Immunity by Vitamin D.” Nutrients vol. 7,10 8251-60. 24 Sep. 2015, doi:10.3390/nu7105392
- Martineau, Adrian R., et al. “Vitamin D Supplementation to Prevent Acute Respiratory Tract Infections: Systematic Review and Meta-Analysis of Individual Participant Data.” BMJ, Feb. 2017, p. i6583. DOI.org (Crossref), https://doi.org/10.1136/bmj.i6583.
- Luxwolda, Martine F., et al. “Traditionally Living Populations in East Africa Have a Mean Serum 25-Hydroxyvitamin D Concentration of 115 Nmol/l.” British Journal of Nutrition, vol. 108, no. 9, Nov. 2012, pp. 1557–61. DOI.org (Crossref), https://doi.org/10.1017/S0007114511007161.
